A case study from back in 2022, looking at some of the work we did across Herefordshire PCN’s. We developed our own PHM tool based on primary care data and worked with subject matter experts to turn the data into actionable insights and ultimately, interventions.
Interestingly, this was the starting point for our current PHM tool that we still use with our customers – albeit it has evolved a bit since then 😊
“How can data be better used to identify health inequalities and deprivation? Herefordshire Primary Care Analytics Team has been working with Herefordshire Place to create a population health management (PHM) tool that would identify inequalities, lead to better health outcomes for patients and improve their wellbeing.”
The need for flexible data
Leaders across the Herefordshire area tended to only know their own organisations and did not have a wider picture of what was going on in the population. Often, data that was being used for decision-making purposes was 12 months out of date, or the 2011 Census had to be relied upon. Data analysts felt there was not enough flexibility in the data they had access to.
The National Contract Direct Enhanced Service (DES), which sets out core requirements and entitlements for a PCN and provides funding and investment, has a particular specification on inequalities. This provided the motivation for using data more cleverly and collaboratively across the 5 PCNs in the area.
“We realised we had acute data such as frequent attenders, but we didn’t have in-depth information available on inequalities and deprivation,” says Conor Price, Chief Analyst, Herefordshire and Worcestershire PCNs. “If we took the raft of data from general practice and built it in such a way that people could find it, people would be able to test out hypotheses, for example if pre-diabetes was a particular issue in a certain deprived area.”
How the PHM tool was developed and how it works
It was this idea that led to the first iteration of the PHM tool, which was called Priority Finder. It meant the data team had to input the data to identify certain cohorts of patients that could be helped. However, it was quickly decided it would be much more useful if people could do it themselves, play with the tool and get the numbers they needed.
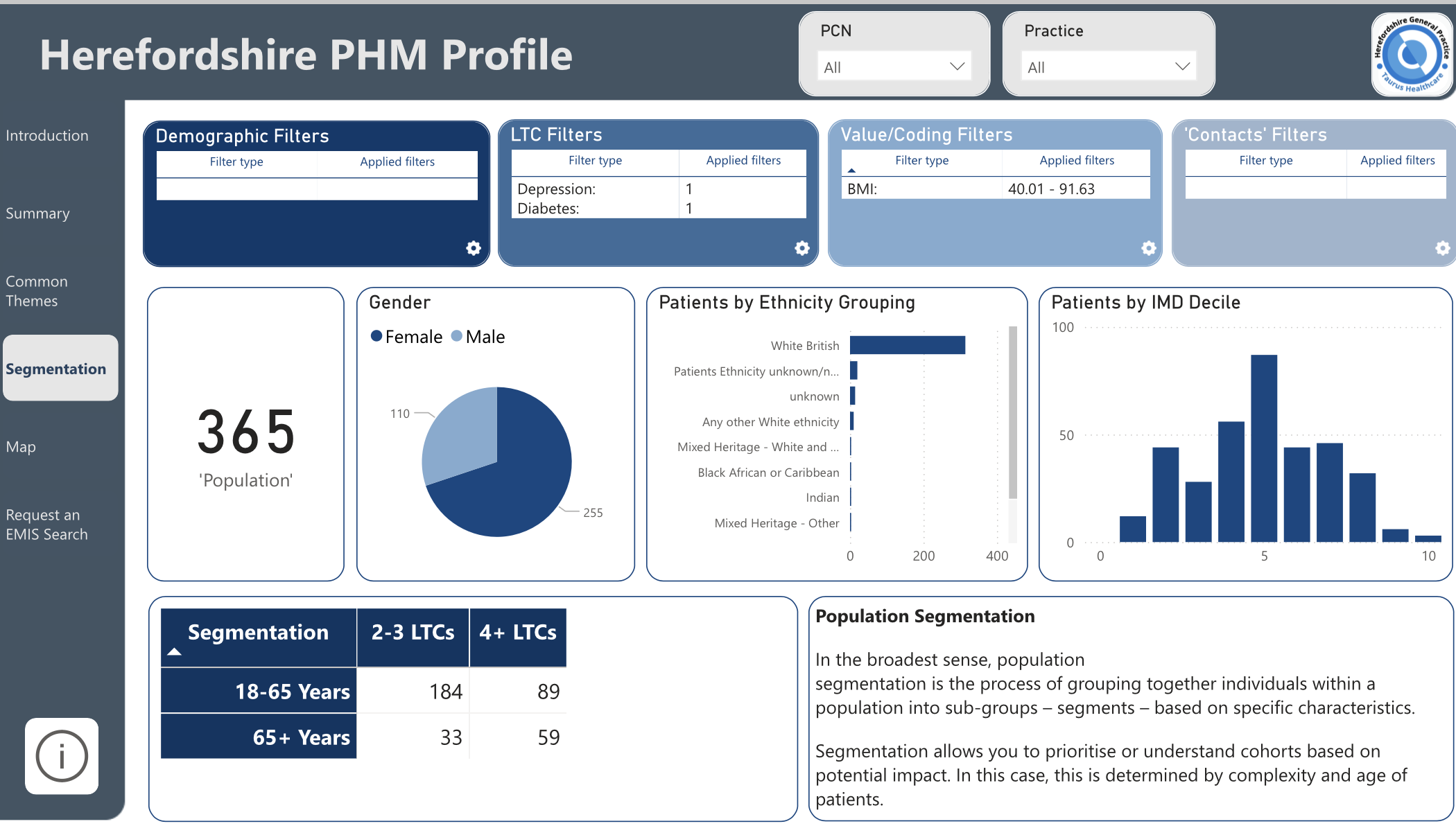
Conor says: “We spent time with each of the 5 PCNs and went through what they were trying to tackle in inequalities, how they were going to identify the cohort of patients and what they wanted to look at. Say they wanted to look at patients who had high blood pressure, no GP contacts and no health check and lived in a deprived area, we were able to do that in front of them, and maybe tell them they had 500 in their PCN – and there are the patients you can make an intervention with.”
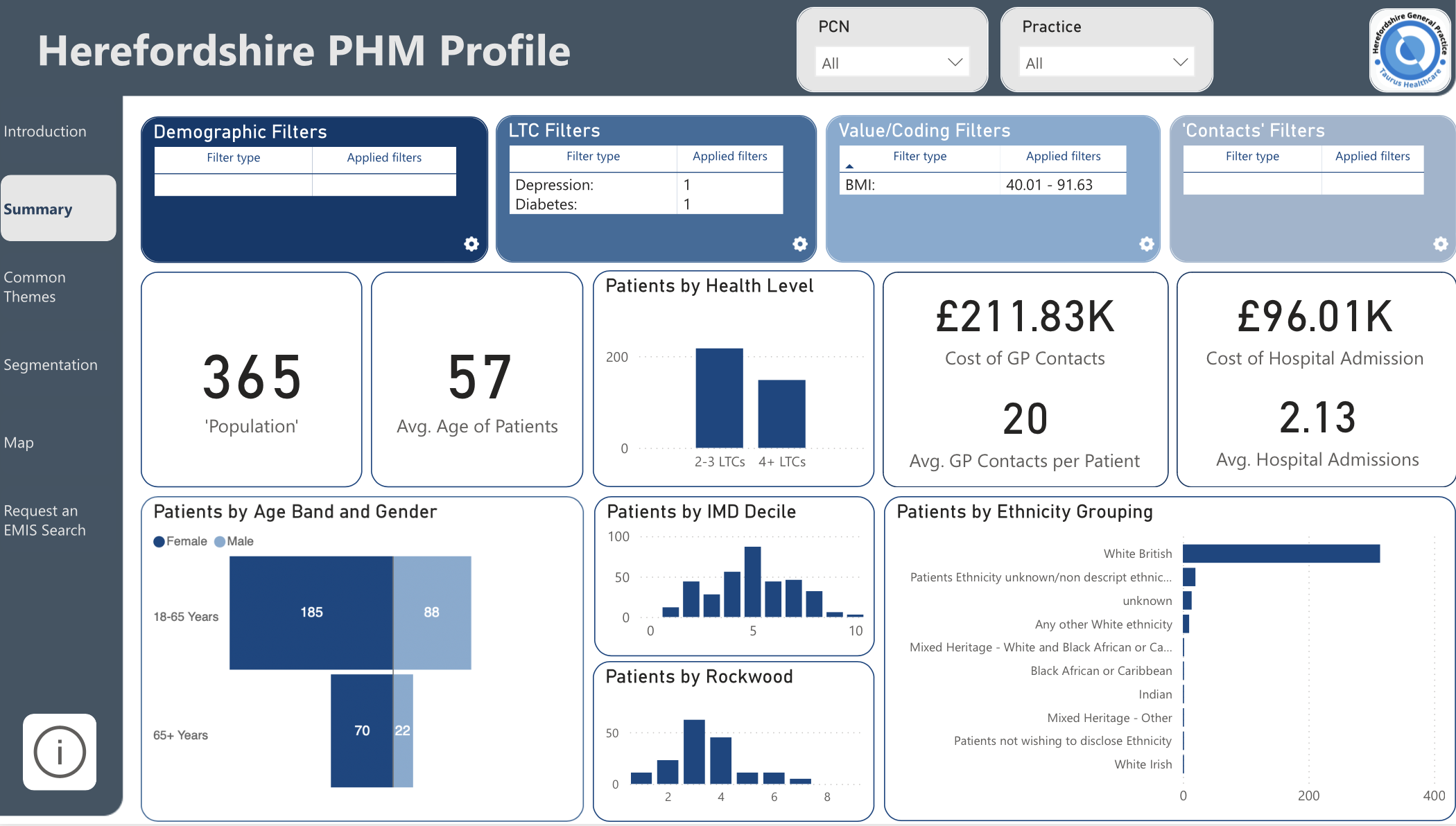
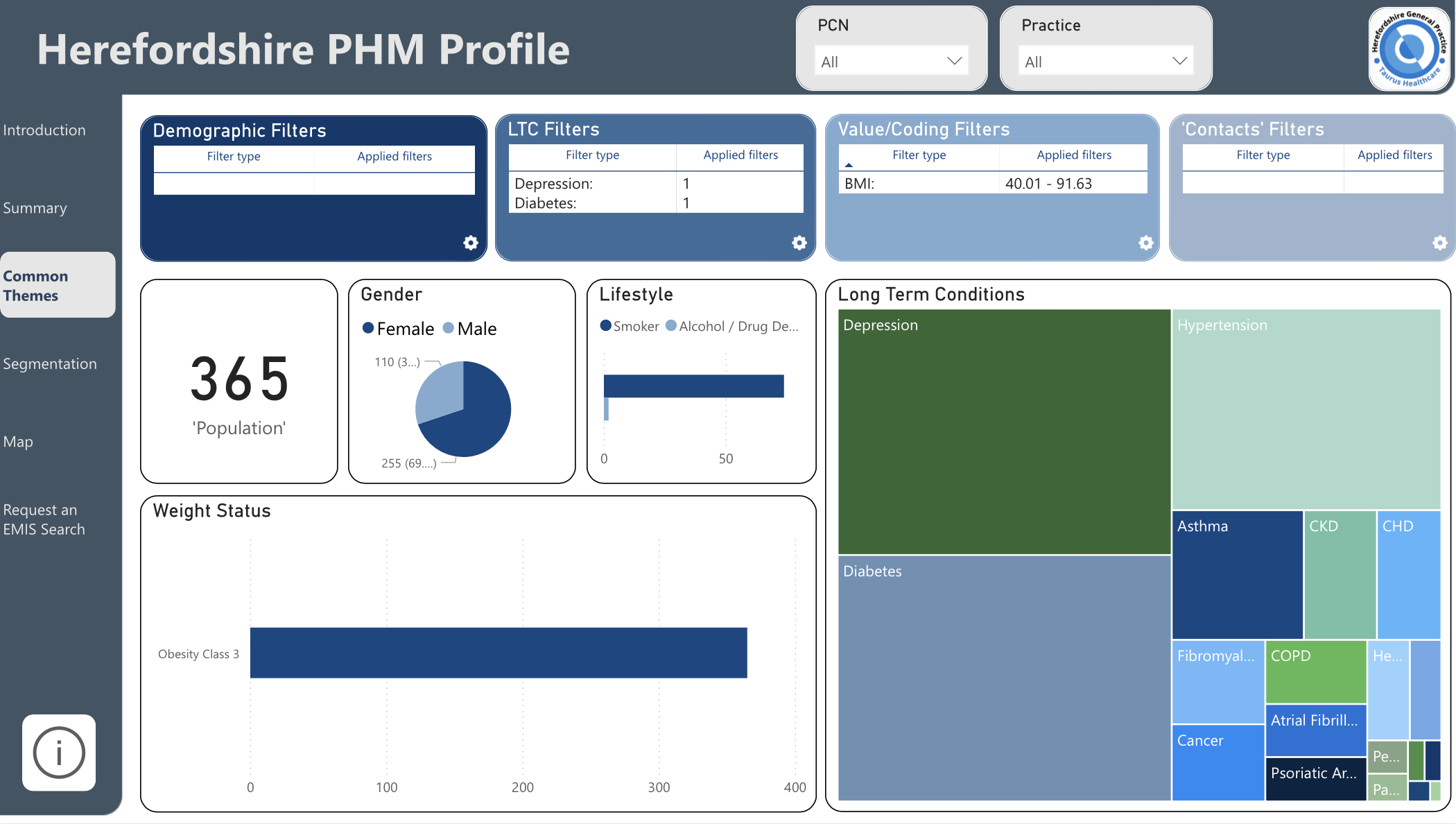
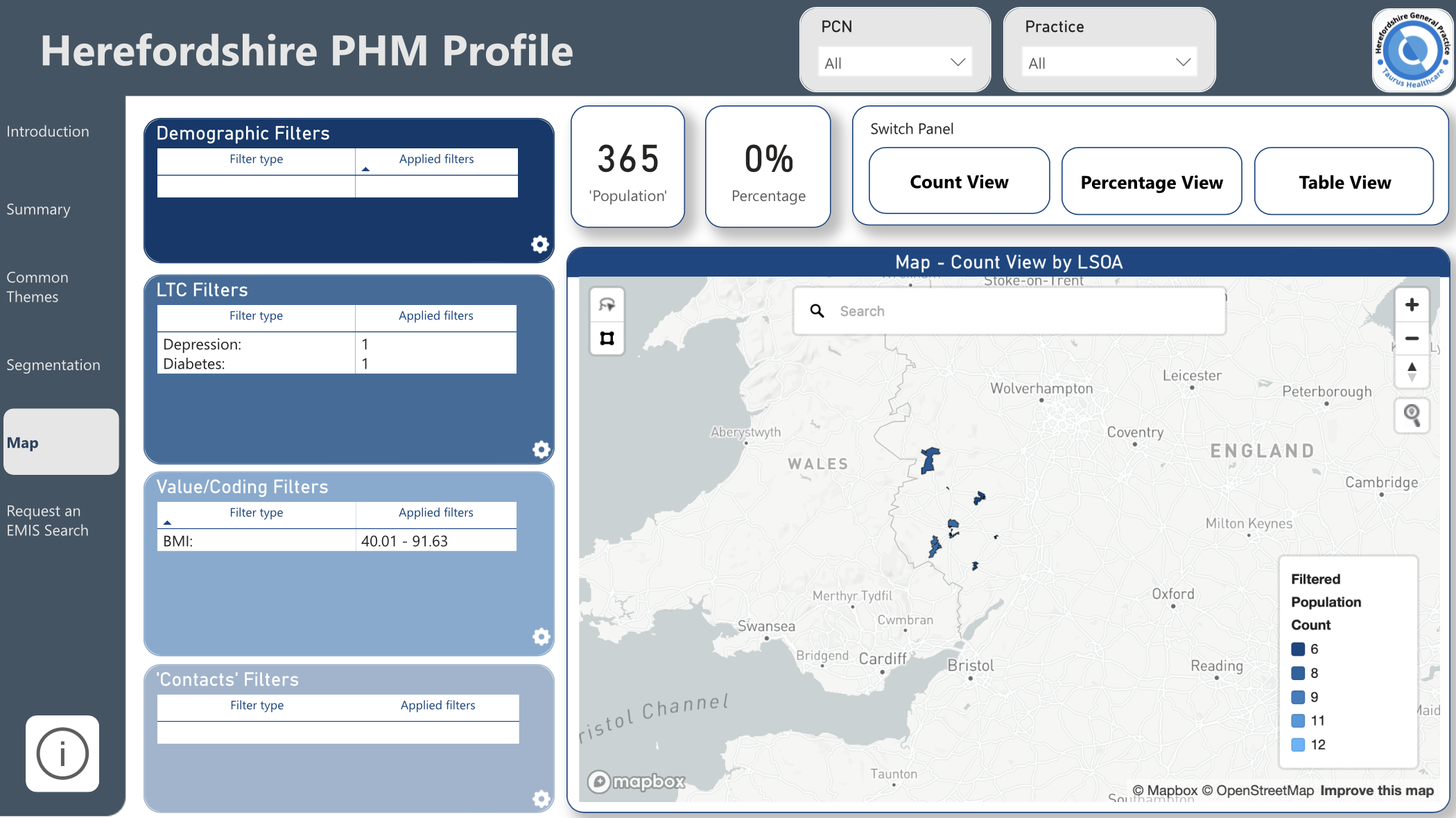
And that is what the PHM tool that Conor and his team built looks like today. It is interactive and allows users to easily drill down into specific areas of the 200,000 people who live in Herefordshire. At a glance, users can see the cost of GP contacts and hospital admissions for different deciles, age groups, genders, ethnicities and more. And within those groups it will also show the average GP contacts and the average medication courses taken. It will also display common themes, for instance which conditions are most prevalent within certain brackets. The data can be repeatedly refined, by adding in additional factors to identify groups that can be targeted with interventions.
Real-world uses
Deborah Humphries, Primary Care Information Lead, explained how the PHM tool data was informing work around unvaccinated patients. She described how one of the PCN Analysts, wanted to look for patients with high BMI, anxiety or depression and no Covid vaccinations. “We identified a good number for them to go and reach out to”. The PCN Analyst went back to the practices to ensure they weren’t on the palliative register and that they were appropriate for the practices to contact to offer the patients some virtual group sessions, and they hope to do in-person sessions too”.
“The ultimate aim is to vaccinate the unvaccinated and engage them in general practice. A lot of the unvaccinated have no contact with general practices whatsoever. We’re trying to reach out to those that feel like they don’t need the vaccinations. It’s still ongoing and patients are still being contacted.”
Gillian Pearson, Head of PCN Development and Partnerships, described another application of the tool where a range of services came together. One PCN looked for cohorts of patients who had high contact with GPs and decided to focus on patients with fibromyalgia and a BMI greater than 30. “They’ve written to the 96 patients they have identified in that cohort and offered them a series of education sessions either online or face-to-face where they have a different session each week, starting with developing a personal care plan,” says Gillian. It includes sessions with dieticians, social prescribers, expert patients and Active Herefordshire and Worcestershire, as well as managing pain, health and wellbeing. The sessions are ongoing, but Gillian said so far the feedback is ‘absolutely phenomenal’. She added: “What we’re hearing is they have never been given information on fibromyalgia on how to manage it before and now they finally have contact details for a network of people they can call on for support. And what we’ve found is patient contacts have reduced and their activation and confidence levels have increased.” By default, there is a cost-saving linked to this.
A similar use of the data elsewhere resulted in a PCN working with the council’s healthy lifestyle and training service to develop six confidence sessions for people with prediabetes and a BMI of 30 or more who had not engaged with other pre-diabetes education support and have anxiety. At the end of their sessions they receive a referral to the National Diabetes Prevention Programme for longer-term support.
Clinical understanding and the value of data going forward
Gillian believes one of the big impacts that population data analysis has had is clinicians understanding the benefit and value of a wellbeing team. “Because clinicians have been involved in helping us find the groups, they understand why they are doing that and have been really engaged,” she says. “There is genuine excitement that we are working with the right patients to make an actual impact and change some of that behaviour positively for patients because they feel better supported.”
And Conor believes the PHM tool will continue to grow in value as its usage increases. The team is already getting more queries as PCNs get used to spending time using it and they find cohorts of patients they want to focus on. “What we have seen is from a starting point where they submitted plans, to actually using the tool and finding out where they can make an impact as they are growing, what they are considering about inequalities is growing so they are coming back and asking us to build a search around that,” he says. The creation of a centralised team of analysts means they are sharing things, work is not duplicated and they can best show how this tool can be used to understand patients in a different way. Conor added: “What it’s demonstrated more than anything is that PCNs value the use of data.”
– Ends –
Date produced: 22/08/2022
Writer: Katherine Hollisey
Type of work: Case study